Subject Emergency & Critical Care
april
Course Details
Week 1 Approach to the Caesarean Patient Brief overview of parturition Complications of parturition Caesarean section Learning objectives After completion of this week,
Course Details
Week 1
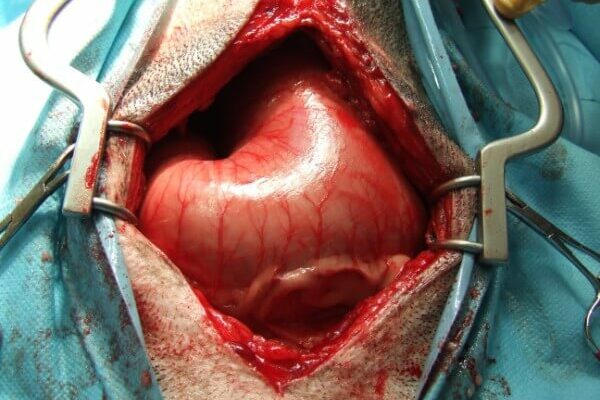
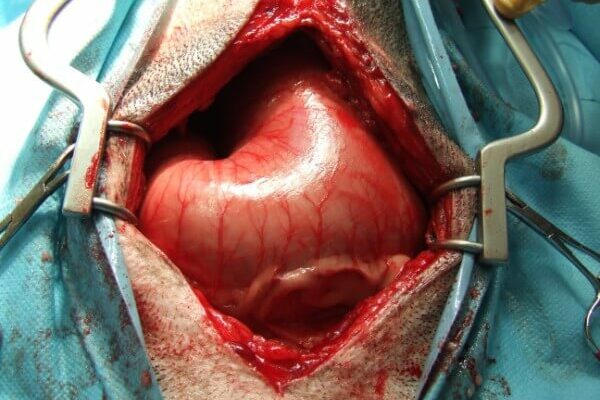
Approach to the Caesarean Patient
Brief overview of parturition
Complications of parturition
Caesarean section
Learning objectives
After completion of this week, participants should be able to:
Explain complications that might occur in parturition
Explain the reasons for intervening in these cases in order to perform a C section
Understand nursing of the caesarean patient
Week 2
The GDV Patient
Physiology of GDV
Diagnosis
Stabilisation of the GDV
Anaesthesia considerations
Post-operative nursing
Learning objectives
After completion of this week, participants should be able to:
Understand the physiology of a GDV and list some of the common risk factors associated with this condition
Describe how a GDV is diagnosed and which tests can help us to identify this condition in the emergency patient
List the common stabilisation techniques in the emergency patient including management of shock and commonly used gastric decompression techniques
Discuss anaesthesia considerations and how to make the patient a safe candidate for surgery
Describe the nursing considerations for the post-operative GDV case and the factors which need to be included in the care plan of the hospitalised patient
Week 3
Nursing the Septic Abdomen Patient
What are SIRS and sepsis?
Recognising sepsis
The use of diagnostic tools in the veterinary practice to help recognise a septic abdomen
Nursing management of a septic abdomen
Learning objectives
After completion of this week, participants should be able to:
Describe SIRS and sepsis and the difference between them
Understand how to recognise sepsis in veterinary patients
List the different tests we have available in practice that can be used to help identify a septic abdomen
Explain how patients with a septic abdomen can best be nursed in practice, pre-, peri and post operatively
Week 4
Haemoabdomen
Physiology of haemoabdomen
Diagnosis
Stabilisation of the haemoabdomen
Anaesthesia considerations
Post-operative nursing
Learning objectives
After completion of this week, participants should be able to:
Understand the physiology of a haemoabdomen and list some of the common causes associated with this condition
Describe how a haemoabdomen is diagnosed and which tests can help us to identify this condition in the emergency patient
List the common stabilisation techniques in the emergency patient including management of shock
Discuss anaesthesia considerations and how to make the patient a safe candidate for surgery
Describe the nursing considerations for the post-operative haemoabdomen case and the factors which need to be included in the care plan of the hospitalised patient
The course will be fully tutored by Elle Haskey and Katie Gray and will consist of 10 hours of CPD given in various formats, including tutorials, tasks, case studies, forum discussions and quizzes. This course is tutored for 4 weeks, followed by a two week extension of untutored ‘catch up’ time, before the course officially ends.
All delegates will then have unlimited lifetime access to the learning material for future reference
Time
April 29 (Monday) - May 24 (Friday)
Location
Online
Speakers for this event
-
Elle Haskey
Elle Haskey
BSc(hons), VTS(ECC) VPAC A1, RVN
HEAD EMERGENCY AND CRITICAL CARE NURSE, ROYAL VETERINARY COLLEGE
BSc(hons), VTS(ECC) VPAC A1, RVN
-
Katie Gray
Katie Gray
Dip AVN, RVN
SENIOR EMERGENCY AND CRITICAL CARE NURSE, ROYAL VETERINARY COLLEGE
Dip AVN, RVN
may
Course Details
Week 1 Approach to the Caesarean Patient Brief overview of parturition Complications of parturition Caesarean section Learning objectives After completion of this week,
Course Details
Week 1
Approach to the Caesarean Patient
Brief overview of parturition
Complications of parturition
Caesarean section
Learning objectives
After completion of this week, participants should be able to:
Explain complications that might occur in parturition
Explain the reasons for intervening in these cases in order to perform a C section
Understand nursing of the caesarean patient
Week 2
The GDV Patient
Physiology of GDV
Diagnosis
Stabilisation of the GDV
Anaesthesia considerations
Post-operative nursing
Learning objectives
After completion of this week, participants should be able to:
Understand the physiology of a GDV and list some of the common risk factors associated with this condition
Describe how a GDV is diagnosed and which tests can help us to identify this condition in the emergency patient
List the common stabilisation techniques in the emergency patient including management of shock and commonly used gastric decompression techniques
Discuss anaesthesia considerations and how to make the patient a safe candidate for surgery
Describe the nursing considerations for the post-operative GDV case and the factors which need to be included in the care plan of the hospitalised patient
Week 3
Nursing the Septic Abdomen Patient
What are SIRS and sepsis?
Recognising sepsis
The use of diagnostic tools in the veterinary practice to help recognise a septic abdomen
Nursing management of a septic abdomen
Learning objectives
After completion of this week, participants should be able to:
Describe SIRS and sepsis and the difference between them
Understand how to recognise sepsis in veterinary patients
List the different tests we have available in practice that can be used to help identify a septic abdomen
Explain how patients with a septic abdomen can best be nursed in practice, pre-, peri and post operatively
Week 4
Haemoabdomen
Physiology of haemoabdomen
Diagnosis
Stabilisation of the haemoabdomen
Anaesthesia considerations
Post-operative nursing
Learning objectives
After completion of this week, participants should be able to:
Understand the physiology of a haemoabdomen and list some of the common causes associated with this condition
Describe how a haemoabdomen is diagnosed and which tests can help us to identify this condition in the emergency patient
List the common stabilisation techniques in the emergency patient including management of shock
Discuss anaesthesia considerations and how to make the patient a safe candidate for surgery
Describe the nursing considerations for the post-operative haemoabdomen case and the factors which need to be included in the care plan of the hospitalised patient
The course will be fully tutored by Elle Haskey and Katie Gray and will consist of 10 hours of CPD given in various formats, including tutorials, tasks, case studies, forum discussions and quizzes. This course is tutored for 4 weeks, followed by a two week extension of untutored ‘catch up’ time, before the course officially ends.
All delegates will then have unlimited lifetime access to the learning material for future reference
Time
April 29 (Monday) - May 24 (Friday)
Location
Online
Speakers for this event
-
Elle Haskey
Elle Haskey
BSc(hons), VTS(ECC) VPAC A1, RVN
HEAD EMERGENCY AND CRITICAL CARE NURSE, ROYAL VETERINARY COLLEGE
BSc(hons), VTS(ECC) VPAC A1, RVN
-
Katie Gray
Katie Gray
Dip AVN, RVN
SENIOR EMERGENCY AND CRITICAL CARE NURSE, ROYAL VETERINARY COLLEGE
Dip AVN, RVN

Course Details
Week 1 Monitoring Modalities There are many advanced monitoring tools and nursing interventions that can be used in our patients, however, a key part of this is
Course Details
Week 1
Monitoring Modalities
There are many advanced monitoring tools and nursing interventions that can be used in our patients, however, a key part of this is deciding when it is appropriate to employ them. We will discuss and compare different monitoring tools that we have available, including:
Blood pressure monitoring – invasive versus non-invasive
Central venous pressure
ECG
Blood gases – venous versus arterial
We will also explore when these monitoring tools may be beneficial compared with when their use might be contraindicated.
Learning objectives
After completion of this week, participants should be able to:
Determine which patients would benefit from more intensive monitoring
Understand how to conduct each kind of monitoring and explain the information we can obtain
Understand the difference between arterial blood pressure monitoring and central venous pressure
Understand the complications of using the more invasive monitoring tools
Week 2
Tubes and Drains
Various tubes and drains are commonly used in critically ill ICU patients, and it is vital we understand how to manage these safely and effectively. We will look at a variety of different tubes and drains including Jackson Pratt drains and active grenades, thoracic tubes, tracheostomy tubes and pericardiocentesis catheters among others.
Learning objectives
After completion of this week, participants should be able to:
Understand the different drains and their functions
Safely manage and nurse patients with various types of tubes
Understand the complications that may occur with various interventions
Confidently troubleshoot drain management
Week 3
Cardiovascular Support
Sometimes fluids just aren’t enough! There are a variety of issues we can encounter with our critically ill patients and cardiovascular support and monitoring becomes an important aspect of the RVN’s role. We will look at the different causes of cardiovascular instability and how we can address those including the use of vasopressors and inotropes.
Learning objectives
After completion of this week, participants should be able to:
Understand the methods of monitoring that can assist with determining both low and high-volume states
Identify cases where the use of vasopressors and inotropes are indicated
Explain the different conditions that lead to changes in cardiovascular function
Understand the ECG assessment and recognise the main life threatening abnormalities
Week 4
Constant Rate Infusions
Constant rate infusions are commonly used in the ICU, and it is really useful for RVN’s to be able to calculate these dosages. Whilst the maths can sometimes seem baffling, if you understand the basics, it is a very useful skill. CRIs are very beneficial for many of our patients and are attainable in any practice with an infusion pump.
Learning objectives
After completion of this week, participants should be able to:
Calculate ANY CRI from scratch!
Understand the benefits and issues associated with use of CRIs
Understand multimodal analgesia options for critically ill patients
The course will be fully tutored by Kath Howie and will consist of 10 hours of CPD and will be provided in various formats, including tutorials, tasks, case scenarios, forum discussions and quizzes. This course is tutored for 4 weeks, followed by a two week extension of untutored ‘catch up’ time, before the course officially ends.
All delegates will then have unlimited lifetime access to the learning material for future reference
Time
May 20 (Monday) - June 14 (Friday)
Location
Online
Speaker
Kath HowieVTS (ECC), RVN Principal Nurse Manager, Vets Now
june

Course Details
Week 1 Monitoring Modalities There are many advanced monitoring tools and nursing interventions that can be used in our patients, however, a key part of this is
Course Details
Week 1
Monitoring Modalities
There are many advanced monitoring tools and nursing interventions that can be used in our patients, however, a key part of this is deciding when it is appropriate to employ them. We will discuss and compare different monitoring tools that we have available, including:
Blood pressure monitoring – invasive versus non-invasive
Central venous pressure
ECG
Blood gases – venous versus arterial
We will also explore when these monitoring tools may be beneficial compared with when their use might be contraindicated.
Learning objectives
After completion of this week, participants should be able to:
Determine which patients would benefit from more intensive monitoring
Understand how to conduct each kind of monitoring and explain the information we can obtain
Understand the difference between arterial blood pressure monitoring and central venous pressure
Understand the complications of using the more invasive monitoring tools
Week 2
Tubes and Drains
Various tubes and drains are commonly used in critically ill ICU patients, and it is vital we understand how to manage these safely and effectively. We will look at a variety of different tubes and drains including Jackson Pratt drains and active grenades, thoracic tubes, tracheostomy tubes and pericardiocentesis catheters among others.
Learning objectives
After completion of this week, participants should be able to:
Understand the different drains and their functions
Safely manage and nurse patients with various types of tubes
Understand the complications that may occur with various interventions
Confidently troubleshoot drain management
Week 3
Cardiovascular Support
Sometimes fluids just aren’t enough! There are a variety of issues we can encounter with our critically ill patients and cardiovascular support and monitoring becomes an important aspect of the RVN’s role. We will look at the different causes of cardiovascular instability and how we can address those including the use of vasopressors and inotropes.
Learning objectives
After completion of this week, participants should be able to:
Understand the methods of monitoring that can assist with determining both low and high-volume states
Identify cases where the use of vasopressors and inotropes are indicated
Explain the different conditions that lead to changes in cardiovascular function
Understand the ECG assessment and recognise the main life threatening abnormalities
Week 4
Constant Rate Infusions
Constant rate infusions are commonly used in the ICU, and it is really useful for RVN’s to be able to calculate these dosages. Whilst the maths can sometimes seem baffling, if you understand the basics, it is a very useful skill. CRIs are very beneficial for many of our patients and are attainable in any practice with an infusion pump.
Learning objectives
After completion of this week, participants should be able to:
Calculate ANY CRI from scratch!
Understand the benefits and issues associated with use of CRIs
Understand multimodal analgesia options for critically ill patients
The course will be fully tutored by Kath Howie and will consist of 10 hours of CPD and will be provided in various formats, including tutorials, tasks, case scenarios, forum discussions and quizzes. This course is tutored for 4 weeks, followed by a two week extension of untutored ‘catch up’ time, before the course officially ends.
All delegates will then have unlimited lifetime access to the learning material for future reference
Time
May 20 (Monday) - June 14 (Friday)
Location
Online
Speaker
Kath HowieVTS (ECC), RVN Principal Nurse Manager, Vets Now
Course Details
Week 1 Vascular Access Indications for IV placement Different types of IV catheter Different placement techniques IV catheter management Complications Learning objectives After completion of this week, participants should be able
Course Details
Week 1
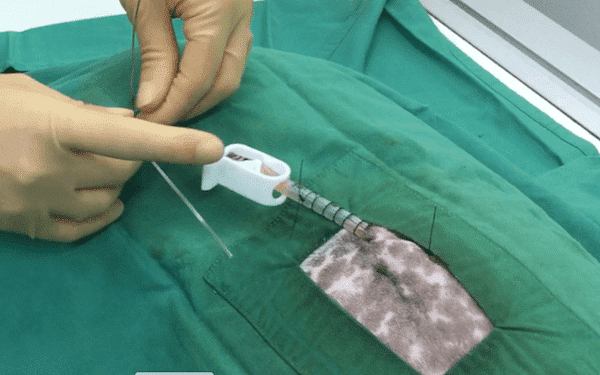
Vascular Access
Indications for IV placement
Different types of IV catheter
Different placement techniques
IV catheter management
Complications
Learning objectives
After completion of this week, participants should be able to:
List the indications and contraindications for IV catheter placement
Understand the difference between peripheral and central venous catheterisation
Describe the different IV catheter options currently on the veterinary market and their placement technique
Discuss how to manage IV catheters – both peripheral and central
Describe the common complications associated with IV catheters and how to minimise them
Week 2
Urinary Catheters
Indications for placing urinary catheters
Different types of urinary catheters
Placement of urinary catheters
Urinary catheter management
Complications
Learning objectives
After completion of this week, participants should be able to:
List the indications and contraindications for urinary catheter placement
Describe the different urinary catheter options currently for veterinary use
Explain how urinary catheters are placed
Discuss how to manage urinary catheters in practice
Describe the common complications associated with urinary catheters
Week 3
Chest Drains
When chest drains are placed
Different types of chest drain
Different placement techniques
Chest drain management
Complications
Learning objectives
After completion of this week, participants should be able to:
List the indications and contraindications for chest drain placement
Describe the different chest drain options currently on the veterinary market and their placement techniques
Explain how to drain the chest drain and what options are available should the patient have a continuous pneumothorax
Discuss how to manage the chest drain and how to identify a drain that is ready for removal
Describe the common complications associated with chest drains and how to minimise them
Week 4
Tracheostomy Tubes
Indications for tracheostomy tube placement
Different types of tracheostomy tubes
Placement of tracheostomy tubes
Management of tracheostomy tubes
Complications
Learning objectives
After completion of this week, participants should be able to:
List the indications and contraindications for placing tracheostomy tubes
Understand the different types of tracheostomy tubes available for veterinary use
Describe how tracheostomy tubes are placed
Explain how to manage tracheostomy tubes in situ
Describe the common complications associated with tracheostomy tubes in practice
The course will be fully tutored by Elle Haskey and Katie Gray, and will consist of 10 hours of CPD given in various formats, including tutorials, tasks, case studies, forum discussions and quizzes. This course is tutored for 4 weeks, followed by a two week extension of untutored ‘catch up’ time, before the course officially ends.
All delegates will then have unlimited lifetime access to the learning material for future reference
Time
june 3 (Monday) - 28 (Friday)
Location
Online
Speakers for this event
-
Elle Haskey
Elle Haskey
BSc(hons), VTS(ECC) VPAC A1, RVN
HEAD EMERGENCY AND CRITICAL CARE NURSE, ROYAL VETERINARY COLLEGE
BSc(hons), VTS(ECC) VPAC A1, RVN
-
Katie Gray
Katie Gray
Dip AVN, RVN
SENIOR EMERGENCY AND CRITICAL CARE NURSE, ROYAL VETERINARY COLLEGE
Dip AVN, RVN
july

Course Details
Week 1 Transfusion Medicine This week we will look at indications for packed red cell and whole blood transfusions, in both cats and dogs, in the acute
Course Details
Week 1
Transfusion Medicine
This week we will look at indications for packed red cell and whole blood transfusions, in both cats and dogs, in the acute emergency setting. The nurse’s role is vital in this field, including preparing the recipient, blood typing, cross matching and monitoring the recipient. We will cover common reasons for transfusion and patient specific nursing concerns, as well as indications for auto transfusion and xenotransfusion. Common coagulopathies will also be discussed, along with indications for the use of plasma products in small animal patients.
Learning objectives
After completion of this week, participants should be able to:
Select the correct blood product for the individual patient
Understand the monitoring these patients require and patient specific concerns
Explain the different transfusion reactions that can occur and how they are avoided and treated
List the indications for auto transfusion and xenotransfusion
Describe the main coagulopathies we encounter and the treatment options available
Week 2
Acute Kidney Injury
Acute kidney injury is a relatively common presentation in emergency and critical care, however, it can occur for a variety of reasons. This week will look at the conditions that lead to acute kidney injury and how we reach that diagnosis. We will look at treatment options including reviews of the evidence bases in terms of patients that are anuric. The nursing role in these patients is multi- faceted and it is vital we can monitor and nurse these patients effectively.
Learning objectives
After completion of this week, participants should be able to:
Understand the different reasons that AKI develops, including post-surgery, toxin related and obstruction of the urinary tract
Understand the monitoring and nursing requirements of these patients including fluid therapy, acid-base status and how we recognize when they are deteriorating
Explain how we manage anuric patients including evidence reviews of methods to force diuresis
Understand the basics of peritoneal and haemodialysis for these patients and the indications
Week 3
Diabetic Ketoacidosis
DKA is a complex disorder that can be life threatening for our patients, and the nursing team play a large role in the management and recovery of these patients. There are multiple considerations in nursing a patient with DKA that go well beyond administering insulin. We will review common reasons for a patient to develop this endocrine disorder as well as acid- base and electrolyte abnormalities we may see.
These patients need intensive monitoring including repeated blood work so we will discuss how to minimize the impact of this on their welfare. There will also be discussion on the different approaches to administration of insulin and ongoing management of these cases when they are discharged home.
Learning objectives
After completion of this week, participants should be able to:
Recognise the concurrent conditions that may lead to difficulty stabilizing the DKA patient
Understand how we reach the diagnosis and the treatment priorities for these patients
Understand the different approaches to insulin administration as well as the pros and cons of each method
Explain how to prioritise appropriate monitoring for these patients
Week 4
Acute Pancreatitis
The pancreatitis patient is a common presentation to any practice. It is an inflammatory condition that can be classed from mild to severe. We will focus on the nursing care and assessment of the patients requiring hospitalisation for management. Whilst we often consider these patients as just needing a couple of days of supportive care, there are some serious complications that can occur and contribute to mortality.
Learning objectives
After completion of this week, participants should be able to:
Understand common aetiologies in dogs and cats
Review pain management options including drug types and routes of administration
Discuss nutritional support options
Identify complications including development of SIRS
Week 5
Acute Respiratory Distress
These patients present many challenges to us in practice and need some special consideration in terms of monitoring and nursing care. We will look at recognition of the patient in respiratory distress, the potential causes, and our priorities for treatment. We will review the monitoring tools that may be beneficial and our approach to stabilising these patients.
Learning objectives
After completion of this week, participants should be able to:
Prioritise stabilisation techniques based on patient presentation
Determine which method of oxygen supplementation is most appropriate for specific patients
Appreciate the management of patients in brachycephalic crisis
Understand the different approaches to diagnostics and monitoring for these very fragile patients
Week 6
Addisonian Crisis
Known as the “great pretender”, Addison’s disease leads to a potentially life-threatening situation when the patient goes into crisis. Whilst electrolyte abnormalities are present in a typical Addisonian we can see no electrolyte changes in atypical cases. The patient with an Addison’s crisis has multiple abnormalities which we need to monitor and correct. Consideration of management options for these patients as well as resolving the crisis will all be discussed.
Learning objectives
After completion of this week, participants should be able to:
Understand the aetiology, common clinical signs, and effects of this complex disorder
Identify and differentiate a patient that has Addison’s disease, with a patient in an Addisonian crisis
Understand the nursing considerations for these patients in the hospital environment, and appreciate the impact stress hormones have
Identify priorities for treatment and ongoing management
This course will be fully tutored by Kath Howie and will consist of 15 hours of CPD given in various formats, including tutorials, tasks, case studies, forum discussions and quizzes. This course is tutored for 6 weeks, followed by a two week extension of untutored ‘catch up’ time, before the course officially ends.
All delegates will then have unlimited lifetime access to the learning material for future reference
Time
July 29 (Monday) - September 6 (Friday)
Location
Online
Speaker
Kath HowieVTS (ECC), RVN Principal Nurse Manager, Vets Now
august

Course Details
Week 1 Transfusion Medicine This week we will look at indications for packed red cell and whole blood transfusions, in both cats and dogs, in the acute
Course Details
Week 1
Transfusion Medicine
This week we will look at indications for packed red cell and whole blood transfusions, in both cats and dogs, in the acute emergency setting. The nurse’s role is vital in this field, including preparing the recipient, blood typing, cross matching and monitoring the recipient. We will cover common reasons for transfusion and patient specific nursing concerns, as well as indications for auto transfusion and xenotransfusion. Common coagulopathies will also be discussed, along with indications for the use of plasma products in small animal patients.
Learning objectives
After completion of this week, participants should be able to:
Select the correct blood product for the individual patient
Understand the monitoring these patients require and patient specific concerns
Explain the different transfusion reactions that can occur and how they are avoided and treated
List the indications for auto transfusion and xenotransfusion
Describe the main coagulopathies we encounter and the treatment options available
Week 2
Acute Kidney Injury
Acute kidney injury is a relatively common presentation in emergency and critical care, however, it can occur for a variety of reasons. This week will look at the conditions that lead to acute kidney injury and how we reach that diagnosis. We will look at treatment options including reviews of the evidence bases in terms of patients that are anuric. The nursing role in these patients is multi- faceted and it is vital we can monitor and nurse these patients effectively.
Learning objectives
After completion of this week, participants should be able to:
Understand the different reasons that AKI develops, including post-surgery, toxin related and obstruction of the urinary tract
Understand the monitoring and nursing requirements of these patients including fluid therapy, acid-base status and how we recognize when they are deteriorating
Explain how we manage anuric patients including evidence reviews of methods to force diuresis
Understand the basics of peritoneal and haemodialysis for these patients and the indications
Week 3
Diabetic Ketoacidosis
DKA is a complex disorder that can be life threatening for our patients, and the nursing team play a large role in the management and recovery of these patients. There are multiple considerations in nursing a patient with DKA that go well beyond administering insulin. We will review common reasons for a patient to develop this endocrine disorder as well as acid- base and electrolyte abnormalities we may see.
These patients need intensive monitoring including repeated blood work so we will discuss how to minimize the impact of this on their welfare. There will also be discussion on the different approaches to administration of insulin and ongoing management of these cases when they are discharged home.
Learning objectives
After completion of this week, participants should be able to:
Recognise the concurrent conditions that may lead to difficulty stabilizing the DKA patient
Understand how we reach the diagnosis and the treatment priorities for these patients
Understand the different approaches to insulin administration as well as the pros and cons of each method
Explain how to prioritise appropriate monitoring for these patients
Week 4
Acute Pancreatitis
The pancreatitis patient is a common presentation to any practice. It is an inflammatory condition that can be classed from mild to severe. We will focus on the nursing care and assessment of the patients requiring hospitalisation for management. Whilst we often consider these patients as just needing a couple of days of supportive care, there are some serious complications that can occur and contribute to mortality.
Learning objectives
After completion of this week, participants should be able to:
Understand common aetiologies in dogs and cats
Review pain management options including drug types and routes of administration
Discuss nutritional support options
Identify complications including development of SIRS
Week 5
Acute Respiratory Distress
These patients present many challenges to us in practice and need some special consideration in terms of monitoring and nursing care. We will look at recognition of the patient in respiratory distress, the potential causes, and our priorities for treatment. We will review the monitoring tools that may be beneficial and our approach to stabilising these patients.
Learning objectives
After completion of this week, participants should be able to:
Prioritise stabilisation techniques based on patient presentation
Determine which method of oxygen supplementation is most appropriate for specific patients
Appreciate the management of patients in brachycephalic crisis
Understand the different approaches to diagnostics and monitoring for these very fragile patients
Week 6
Addisonian Crisis
Known as the “great pretender”, Addison’s disease leads to a potentially life-threatening situation when the patient goes into crisis. Whilst electrolyte abnormalities are present in a typical Addisonian we can see no electrolyte changes in atypical cases. The patient with an Addison’s crisis has multiple abnormalities which we need to monitor and correct. Consideration of management options for these patients as well as resolving the crisis will all be discussed.
Learning objectives
After completion of this week, participants should be able to:
Understand the aetiology, common clinical signs, and effects of this complex disorder
Identify and differentiate a patient that has Addison’s disease, with a patient in an Addisonian crisis
Understand the nursing considerations for these patients in the hospital environment, and appreciate the impact stress hormones have
Identify priorities for treatment and ongoing management
This course will be fully tutored by Kath Howie and will consist of 15 hours of CPD given in various formats, including tutorials, tasks, case studies, forum discussions and quizzes. This course is tutored for 6 weeks, followed by a two week extension of untutored ‘catch up’ time, before the course officially ends.
All delegates will then have unlimited lifetime access to the learning material for future reference
Time
July 29 (Monday) - September 6 (Friday)
Location
Online
Speaker
Kath HowieVTS (ECC), RVN Principal Nurse Manager, Vets Now

Course Details
Week 1 Patient Assessment and Triage The concept of triage Preparedness Primary survey Secondary Survey Emergency history Learning objectives After completion of this week, participants should be able to: Understand the triage
Course Details
Week 1
Patient Assessment and Triage
The concept of triage
Preparedness
Primary survey
Secondary Survey
Emergency history
Learning objectives
After completion of this week, participants should be able to:
Understand the triage process and how it can be utilised to prioritise emergency care
Describe how to make their team and environment prepared for when the emergency patient arrives
List how to carry out a primary survey during the initial assessment of the patient
Explain how to carry out a secondary survey assessment in order to list their concerns with the patient
Discuss how to communicate with the client including telephone advice, informed consent and emergency history
Week 2
Shock
Classify shock
Emergency database
Blood pressure
Oxygen therapy
The use of multiparameter monitors
Learning objectives
After completion of this week, participants should be able to:
Identify a patient with shock and classify which type of shock they have
Explain which parameters may be tested during an emergency database and how these can help to identify shock in the emergency room
Understand the physiology of perfusion and ways in which blood pressure can be monitored in the emergency patient
List the different ways that oxygen therapy can be delivered to the emergency patient
Understand the uses and limitations of multiparameter monitors and their role in monitoring perfusion trends
Week 3
Fluid Therapy
Patient assessment
Identifying a fluid deficit or change in volume
What fluids are available
Managing a change in content
Identifying a change in fluid distribution
Learning objectives
After completion of this week, participants should be able to:
Explain how to assess the patient’s fluid status using clinical exam and blood work
Discuss how to create a fluid plan to treat a fluid deficit such as hypovolaemia or dehydration
List what fluid options are available and which fluid might be preferred in which situation
Understand how fluid selection or the fluid plan can be altered to account for an electrolyte abnormality
Describe how to manage the patient with fluid overload or peripheral oedema
Week 4
Neurological Emergencies
Neurological assessment
Coma scoring
Raised intracranial pressure
Seizures
Learning objectives
After completion of this week, participants should be able to:
Describe how to perform a neurological assessment of an emergency patient
Describe how to perform a coma score and understand how these may be used in neurological patients
Understand methods of identifying raised intracranial pressure and the physiology behind this
Recognise a seizuring patient and understand their management, from initial presentation and stabilisation of mild seizures through to the management of a patient in status epilepticus
Week 5
Approach to the Trauma Patient
Assessment of wounds
Wound management
Management of fractures
Other injuries associated with trauma
Analgesia
Learning objectives
After completion of this week, participants should be able to:
Identify different wounds based on the patient history and appearance of the wound
Understand the principles of wound management and common techniques used to flush and debride wounds
Describe how to identify and manage fractures in the trauma patient
List other common injuries associated with trauma and how these should be managed
Implement an analgesia plan for the trauma patient based on pain assessment
Week 6
Common Toxicities
Common toxins seen in emergency practice
Renal toxins
Hepatotoxins
Anticoagulants
Neurotoxins
Learning objectives
After completion of this week, participants should be able to:
Describe the different ways toxins can enter the body
List the most common renal toxins and understand the treatment of these patients
List the most common hepatotoxins and understand the different treatments for each of these
Understand the physiological effects of anticoagulant ingestion and the treatment of these patients
Identify the most common neurotoxins seen in practice and understand the treatment of these patients
The course will be fully tutored by Elle Haskey and Katie Gray and will consist of 15 hours of CPD given in various formats, including tutorials, tasks, case studies, forum discussions and quizzes. This course is tutored for 6 weeks, followed by a two week extension of untutored ‘catch up’ time, before the course officially ends.
All delegates will then have unlimited lifetime access to the learning material for future reference
Time
August 12 (Monday) - September 20 (Friday)
Location
Online
Speakers for this event
-
Elle Haskey
Elle Haskey
BSc(hons), VTS(ECC) VPAC A1, RVN
HEAD EMERGENCY AND CRITICAL CARE NURSE, ROYAL VETERINARY COLLEGE
BSc(hons), VTS(ECC) VPAC A1, RVN
-
Katie Gray
Katie Gray
Dip AVN, RVN
SENIOR EMERGENCY AND CRITICAL CARE NURSE, ROYAL VETERINARY COLLEGE
Dip AVN, RVN